Before I discovered Health At Every Size, my relationship with food and exercise had one mode: will this make me thin or fat?
And that was pretty much it.
There was no “will I truly enjoy this?” There was no “how will this make me feel?”
And there was very little concern for my actual health and well-being outside of the “thin-is-good” / “fat-is-bad” paradigm.
My weight-centric view of eating and exercise became obsessive very quickly…ultimately leading to a variety of disordered eating behaviors, including but not limited to:
- Chronic attempts at under-eating/restriction,
- followed by binge eating,
- weight-cycling (aka “yo-yo dieting”)
- food obsession,
- low self-esteem,
- (A LOT) of emotional eating,
- and generally feeling “crazy” around food.
While I clung tightly to the hope that I could “recover” from diet-binge cycling and still casually try to lose weight,
I was never able to truly heal my relationship with food—including my binge eating behaviors—until I put all the attempts at dieting down and started pursuing “health” in weight-neutral ways.
Ultimately, the core concepts introduced by Health At Every Size (combined with Intuitive Eating and some deeply important self-acceptance work) eventually helped me find the “off-ramp” of the diet-binge cycle.
What is Health At Every Size (HAES)?
Health At Every Size (“HAES”) is a weight-neutral approach to health care that promotes the pursuit of healthful behaviors (like eating vegetables, moving your body, getting enough protein, etc.) for the inherent health benefits of those behaviors, rather than for the explicit purpose of weight manipulation.
For instance, HAES-inclined wellness professionals may suggest that clients move their bodies for the sake of its cardiac or mental health benefits—rather than for the purpose of thinness.
Health At Every Size additionally promotes the pursuit of health outcomes (like balanced blood sugar, blood pressure, heart health, etc.) through the pursuit of healthful behaviors, rather than through the pursuit of weight loss.
For instance, HAES advocates may suggest that patients manage diabetes or heart disease through movement or nutritional therapy, rather than asking patients to lose weight as a proxy for healthy behaviors.
Additionally, Health At Every Size is a grassroots political and social justice movement, advocating for the adoption of weight-neutral health care in all health and wellness spaces.
On that note,
HAES is a movement made up of many different people, voices, and ideas.
I cannot speak for the entire movement—I can only share my own understanding of these concepts, and for the sake of simplicity and efficiency, I’m choosing to distill that understanding down into what I believe are the most crucial introductory points.
Why Health At Every Size (instead of dieting)?
At its most fundamental level,
Health At Every Size is an alternative to our current weight-centric approach to health care—an approach which has been largely proven ineffective.
Below are some reasons why our current weight-centric health care system—meaning, health care that aims to make people thinner as a means to improved health outcomes—doesn’t work and is probably making people sicker long-term.
#1. Diets don’t work.
The Health At Every Size approach was developed in response to an ever-growing body of research showing that diets for weight loss are unsustainable and do not result in improved health outcomes for most people long-term.
You may have heard the statistic thrown around—that 95% (ish) of diets fail over time.
What this statistic actually means is that no peer-reviewed weight loss research—of any kind or by any method—can demonstrate consistent “weight loss success” for more than a small fraction of participants in the long term.
While most people are able to lose weight temporarily through dieting—
typically no more than 5% of research participants (give or take a few points depending on the study) are able to maintain “significant” weight loss—by any method—for more than 3-5 years. More on this here.
These numbers diminish even further in the rare cases that weight loss lasts more than 5 years, and those rare people who DO maintain “long-term, significant” weight loss often exhibit attitudes and behaviors that would be diagnosed as eating disordered in lower-weight people
(i.e. they must stay vigilantly obsessed with food and exercise and not much else—more on this in a moment).
This all to say, most people do not succeed at forcible attempts at weight loss in the long-term—no matter how, or why, they are trying to do so.
While HAES advocates typically reject the idea that “health” should be defined by body size (since many fat people live perfectly healthful lives in the bodies they have, and thin people are not immune to “weight-related” illnesses like heart disease or diabetes),
most agree that it is irrelevant whether or not your personal definition of “health” includes thinness—because there is simply no safe or “proven” method of weight loss that exists when you consider sustainability and long-term probable outcomes.
#2. Diets lead to weight gain.
Additionally, research suggests that forced attempts at weight loss lead to long-term (rebound) weight-gain in about a third of instances.
In other words,
every time you lose weight on a diet—you have about a 30% chance of ending up bigger than when you started, after going through a full diet-rebound cycle.
As it turns out, dieting (or trying to lose weight) is the number one predictor of weight gain over time.
On the flipside, non-dieters—or those practicing HAES and size acceptance—maintain their natural set point weight effortlessly with relative stability over time.
#3. Diets may be unsafe (even for those who are “successful”)
Not only does dieting as a “treatment” for fatness not usually work, but it comes with a long list of side effects—including but not limited to:
binge eating, emotional eating, low self-esteem, food obsession, eating disorders, depression/anxiety, and a wide variety of physical ailments that may result from malnutrition or weight cycling.
Weight cycling—that is, losing weight and gaining it back over and over again—is a known stressor on the body and is associated with some of the same chronic illnesses that are typically blamed on fatness.
Some research suggests that certain negative health outcomes associated with fatness (e.g. diabetes and heart disease) may be a result of chronic yo-yo dieting, or weight cycling, which is disproportionately encouraged in larger-bodied people.
Additionally, the psychological impacts of chronic dieting are bleak—irrespective of maintenance or “success.” Malnutrition and disordered eating are common and serious threats to anyone attempting or maintaining significant weight loss, irrespective of their starting weight.
What “works” about Health At Every Size
While many feel hopeless about their prospects for dieting—worried they are doomed for ill health and disease if they’re unable to achieve or maintain long-term weight loss,
there is an alternative to dieting that is more effective in improving health outcomes AND has fewer side effects—including less binge eating, weight-cycling, and less feeling “crazy” around food.
And this approach is surprisingly simple…
Pursue a healthy lifestyle—including things like eating vegetables, getting regular movement, managing stress or [insert healthy behavior of your choice]
…without worrying about the weight part.
Voila!
There are several reasons why this strategy is more effective (and less harmful) than dieting “for health,” but I’ll review some big ones below for your review.
HAES is more sustainable
As it turns out, people are more likely to sustain healthy behaviors (like eating vegetables, and moving their bodies) when those behaviors are NOT motivated by weight-related goals.
There are a couple of reasons for this—
First off, thinness may motivate people to work out or eat vegetables on “Day One”
…but the second a dieter perceives themselves as “off the wagon,” or becomes frustrated when they don’t get the weight results they were hoping for, they tend to throw in the towel on whatever health behaviors they attached to dieting…until their next diet of course.
On the flipside, health behaviors that are motivated by immediately tangible benefits (e.g. endorphins, better sleep, generally feeling better, etc.) are intrinsically rewarding and are thus more likely to be continued—irrespective of perceived “performance” or judgments of those behaviors.
Secondly, eating restrictions are biologically difficult to maintain—even for the most strong-willed or “motivated” people.
Limiting calories or major macronutrients (e.g. fat, carbs, etc.), which is often encouraged by diets “for weight loss” sends our bodies into starvation mode and our biological instincts quickly rebel—leading to binge eating, rebounding, and other complications of malnutrition (eek!).
While diets tend to focus on taking things out—that is, limiting amounts or types of food consumed—the HAES approach focuses on adding in healthful behaviors, like exercise, vegetables, etc.
Adding “healthful” things into our life is significantly easier for our human brains than taking “unhealthful” things out. After all, we’ve evolved over millions of years to seek food rather than resist it.
When limiting certain food types IS necessary for “health” (e.g. physical allergies, etc.), folks are more likely to succeed long-term—and are less likely to fall into binge eating behaviors—when pursuing these restrictions in a weight-neutral way.
Weight is a flawed indicator of “health”
The second reason that HAES is more effective than weight-centric health strategies, is that not all bodies are genetically “designed” for thinness.
Some people’s healthiest possible weight—the weight they end up at when they’re at the top of their personal “health” game—is higher than current medical BMI “recommendations.”
Advocates of Health At Every Size recognize that bodies—including “healthful” bodies by metabolic standards—naturally occur in a range of sizes.
Some data suggests that more than half of “overweight” people are “metabolically healthy” (meaning healthy blood sugar, blood pressure, cholesterol, etc.) while about a quarter of thin or “normal weight” people have at least two risk factors typically associated with “obesity.”
While our medical system assumes that thin is unilaterally healthy and fat is unilaterally unhealthy, this is a highly flawed assumption—one that is largely based on correlational data and is un-useful in predicting individual health outcomes.
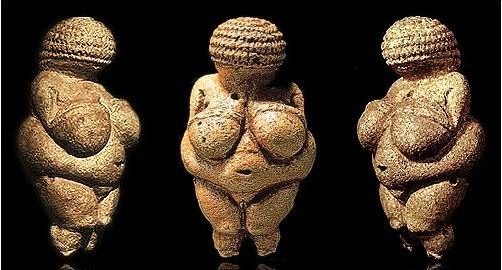
This all to say, naturally occurring body diversity is a thing…and it’s been a thing for thousands of years.
HAES reduces weight-bias in health care settings.
One of the biggest problems with our weight-centric health care system is that it encourages weight-bias in almost every aspect of our medical system.
The existence of weight bias in our medical system is well-documented, and has dangerous (even fatal) implications for larger-bodied people.
For instance, fat people are told to lose weight (aka diet) in response to just about every health problem, ache, or pain, they could possibly present with—while their thin counterparts are treated with actual evidence-based medicine.
It’s not uncommon for serious medical threats (think: tumors, blood clots, broken bones, etc.) to go undetected in larger patients because doctors assume their symptoms (everything from knee-pain to chest pain to trouble breathing) are no more than simple side effects of fatness that would go away if they just lost weight.
Larger bodied patients are viewed by doctors and nurses as “lazy” or “non-compliant” (when diets inevitably don’t work) and patients hesitate to pursue medical care to avoid being shamed and judged for their size.
Higher-weight people are regularly denied medical care—especially surgeries and insurance coverage, “unless/until” they lose weight.
In other words, patients have to WAIT to receive basic medical services until they do something that may not be healthful or possible for them.
WHAT THE ACTUAL F*CK.

Many HAES advocates have pointed out that the only real way to close the “health gap” between larger and thinner bodied people is to eliminate weight-based stigma and oppression in our health care system and throughout the world.
Repairing social inequities that affect health care has thus become a quickly growing priority for the HAES movement. Furthermore, most HAES-aligned organizations (e.g. ASDAH, which currently owns the HAES trademark) center intersectional justice in their activism and extend their mission to promote justice for ALL marginalized groups—including those based on race, gender, accessibility, and others.
“Health At Every Size” Title-Confusion
There are a lot of misunderstandings about HAES—and it’s easy to understand why.
The title is controversial (even amongst HAES and other body-positive activists), simply because it lends itself to gross misunderstanding about what HAES actually is.
Most of what you’ll read about “Health At Every Size” on the internet is a product of simple misunderstanding…so let’s clear up the most common “objection” to the HAES approach once and for all.
OBJECTION: “But fat bodies are unhealthy”
While it seems pretty clear from research that this is NOT unilaterally true—there are plenty of fat people that live long, disease-free lives, and there are plenty of thin people who die from “weight-related” illnesses like diabetes and heart disease—
it’s important to note that HAES advocates are not making ANY claims about what bodies are, or are not, “healthy,” however you may define that term.
HAES advocates are not claiming that “everyone is healthy at every size,” or that “every size is equally healthy” or any version of this sentiment.
HAES advocates are simply promoting a weight-neutral approach to health care—one that focuses on the promotion of healthy behaviors and lifestyles, rather than trying to make people universally thin as a proxy for good health.
In other words, HAES advocates are promoting a more effective way of pursuing health—while warning against the dangers and ineffectiveness of forced weight loss attempts.
Getting Started with Health At Every Size
When you finally come to terms with the realistic prospects of dieting (I know…there may be some mourning involved…), here are some steps that you can take to pursue your happiest, healthiest life in whatever body you’re realistically working with.
#1. Set Weight-Neutral Health Goals (aka “Plan B”).
Instead of obsessively trying to lose weight for years on end with no lasting results,
think about the health or fitness goals that matter to you—the things you think you’ll get through weight loss—and start pursuing those goals directly in the body you have right now.
For instance,
- Do you want to work on mobility? Awesome, let’s do some strength training and stretching…that’ll help whether you lose weight or not.
- Do you want to walk, run, or climb up the stairs more easily? Awesome, let’s get some more cardio in…that will also help whether you lose weight or not.
- Do you want to manage your blood sugar or blood pressure more effectively? Great! Let’s work on getting enough protein and fiber at meals and snack times—a little cardio helps here too!
…all of which helps whether you lose weight or not!
There are loads of things you can do to improve pretty much any “weight-related” health condition…that have nothing to do with diets-that-don’t-work-anyway.
In other words, start thinking about Plan B: weight-neutral actions you can take to achieve the health outcomes you’re looking for…regardless of what happens with your size.
Additionally, set weight-neutral health goals that are reasonable for your unique body and lifestyle.
If a particular form of movement isn’t available to you—for weight or non-weight-related reasons—you have to meet yourself where you are.
Similarly, if a particular dietary change isn’t realistic for economic, lifestyle, mental health or any other reasons—work within your life circumstances rather than against them.
There is no “right” way to do health…and all health pursuits should be realistic, practical and most importantly feel good to the individual pursuing them.
(Otherwise…what’s the point?)
#2. Be okay with what you can’t control.
Recognize that like weight, “health” outcomes are not fully within your control either.
Although focusing on behavioral change is more effective than dieting when it comes to long-term health outcomes—behavioral change itself can only go so far.
When we honestly acknowledge the role of genetics, environment, social inequality, and an infinite number of unknowable factors—it becomes clear that we are only “in control” of a small fraction of our own “health” inputs.
Arguably our own behaviors are not even fully within our control, because our behaviors are impacted by our environment, energy levels, attitudes and beliefs, etc.
This all to say, you can take some of the pressure off yourself.
Despite what most health blogs would have you believe—it’s not all on you, and you don’t get to choose the day you die.
#3. Don’t forget about mental health.
Since there is NO dietary or health choice that will make you immortal—and there is no point in trying if you have to be miserable to achieve it—don’t forget to enjoy life now.
Physical health has little value if you can’t enjoy your life in this moment.
Even if I could “misery” my way into longevity—I’d gladly take a few years off my life if it meant that I could have fun and live well in the years I had, rather than spend my life an anxious, food-obsessed wreck.
Additionally, there is strong research suggesting that people who are relaxed and happy are better protected from a range of illnesses, including heart disease and diabetes.
This all to say—mental health and well-being is an equally important piece of our overall “health” equation.
If your pursuit of physical health is destructive to your mental health—it’s probably not sustainable and almost certainly not worth it.
Find support and resources.
What I’ve shared with you today is the tip of the iceberg of problems associated with a weight-centric (and weight-biased) health care system, and we all need as much help as we can get to manage the shitstorm of problems that result from a culture of widespread fatphobia.
If you’ve had enough of diets-that-don’t-work and are ready to pursue a weight-neutral, body-positive approach to health—seek out support in whatever ways are realistic for you.
 Arm yourself with education—check out the book, Health At Every Size, by Linda Bacon, as well as the Intuitive Eating book to learn core concepts of the “non-diet” approach.
Arm yourself with education—check out the book, Health At Every Size, by Linda Bacon, as well as the Intuitive Eating book to learn core concepts of the “non-diet” approach.
Make sure to review HAES informed blogs like Dances With Fat, for an ongoing conversation about how people of all sizes can pursue weight-neutral health and support people in larger bodies who are suffering at the hands of weight-bias in our culture.
If you’re struggling to let go of dieting, diet-mentality, or are healing from diet-binge cycling, check out my free video training series, which outlines my own binge eating and diet recovery philosophy by clicking here—
(Or better yet, sign up for my group coaching program, the Stop Fighting Food MASTER CLASS!)
Lastly, seek out HAES informed health professionals in your area through the Association for Size Diversity and Health.
ASDAH equips wellness professionals with research and other resources that support a size-inclusive health philosophy, and only accepts members that represent as non-diet, size-inclusive and HAES-informed.
If you’re not already on my email list, make sure to sign up above for HAES-informed, diet-recovery blog posts and support.
Lastly, if this post was helpful to you, I hope you’ll share it on FB so we can get these important distinctions out into the world.